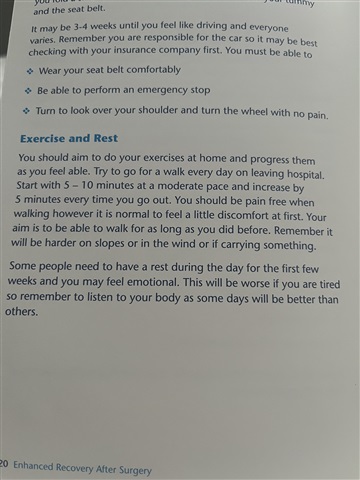
I am 66 yrs old and had a total laparoscopic/vaginal hysterectomy on 9th May. Had a great first week, hardly any pain or painkillers. I feel I may have walked outside a bit much on days 8 and 9, approx 30 minutes each time and had some pain after this. The attached photo from my NHS enhanced recovery booklet recommends 5 to 10 minutes on first day and adding 5 minutes each time you go out, so this would mean half an hour by day six after discharge - see photo below. This now seems in excess of other guidance I have read. I rested a bit more this week (week 2) Went out today, passenger in car for ten mins to town centre, walked ten minutes from car to coffee shop and same on return journey. Experienced pain again on my return home. Naturally I am resting as a result. Would appreciate some guidance on how much I should be walking and on building this up at this stage.
My bowels and bladder were working well week one. This past week my frequency of urination has increased quite significantly. Could this be due to excessive walking? I was tested for a uti and this was clear.
Thank you.
Hi Dolly
I went for short walks when I got home from the hospital and built up slowly, listening to what my body was telling me. A couple of times when I felt better, I did over do it a bit. The following day I had some swelling in my tummy and a lot of fatigue. I also had a few aches and pains.
I would suggest the best thing to do is to give your CNS a call- there should be details on your discharge paperwork and ask for some advice specific to you. I am not sure what may be causing the increased urination and it is something worth mentioning, along with the pain. It is good that your urine test was clear. I wonder if there is some bruising or swelling coming out internally that could be causing this. It may also be due to the inside organs all starting to settle into place after the surgery. Although the surgery was key hole- inside it is still major surgery and you are only at 2 weeks post op. During this time I would think contacting the hospital would be the best plan.
If you would like to talk things through first then please do give the Support Line a call. It is there from 8am-8pm daily.
Resting in the mean time sounds a good thing to do.
Jane
Hi Dolly,
I had a full hysterectomy and everything taken out, two years ago. I didn't see any guidance that looks exactly like this, but I did read plenty of info on what, when and how much to do!
I have a high pain threshhold (which can be an advantage but also can be a disadvantage if I end up doing too much just because I think I can!) but I roughly recall, that I was driving by two weeks after, but was sitting in my car working the pedals at 5 days out, and wondering why they said I had to be able to do an emergency stop as I did the motions and had no probs at all - no pain, no discomfort, etc.
I was walking up and down the ward in the day and a half I was in...every hour I would take a walk past the nurses' station and out to the courtyard and back. When I got home, I was walking my dogs from day one but I would walk about ten minutes, then sit on a bench for a bit, then walk another ten, then bench, and so on and so forth. I just made sure I sat after every ten mins or so of walking.
By the second week after arriving home, I was doing the half hour or so walk without resting. I did at home make sure I was lying on the bed for an hour every three or four hours. (I took 7 weeks off work)- I had to force myself to, but got through a lot of puzzle books and a lot of reading!!
All the guidance I read, said that if you do an activity that causes pain, stop that activity and re-visit it in a few days. Everyone is different, so it's hard for guidance to be applicable to every person in the same way.
Because I don't feel pain much - unless it's very severe - I had no way of telling if I needed to stop an activity and re-visit later, as nothing I did caused me any pain. So I just took it slowly and sensibly, and built up week by week regardless.
If you feel pain after ten minutes, or twenty, rest a bit more for a day and then maybe walk a few minutes less and start building up again. That's what all the advice I read, seemed to be telling me.
The urination, could be because your bladder is coming alive again after a bit of sluggishness caused by the surgery. (They move your bladder around a lot, I'm told.) Once you are healed, at least 6 weeks in but probably 12 weeks to be safe, start doing pelvic floor exercises very gently, and build those up over the coming months. That will help prevent urinary problems in the future, which apparently is a side effect of this surgery. You're supposed to do them for life - I keep forgetting mine!!! but touch wood, I haven't yet after two years had any incontinence issues.
My recovery was similar to Maite’s, but I’d say my tolerance to pain is low. As soon as my catheter was out 6am the following day, I was up out of my hospital bed and didn’t return to it. Every half hour or so I walked up and down the corridor to and from the nurses’ station. As soon as I got home that lunchtime I went for a gentle 5 minute stroll round a local block. The following day I did 2 x 5 min walks, the day afterwards I did two walks but increased one walk to 10 mins, and so on, as I felt able, until I was up to 40-60 minutes per day by 2 weeks post op. I started sitting in my car practising the pedals from day 2 post op, and started going forwards and backwards in our driveway on day 4, and drove half a mile up the road on day 5 so that I could do a short 5-10 min off lead walk with my dog. The week after I drove to my local supermarket (one mile away) to do some shopping. What I used as my guide was listening to my body - which meant pushing myself if I felt up to it, and resting when I needed to. A friend on here ws told by her consultant that you can’t overdo walking as long as you’re listening to your body so she took a walk to her local supermarket 3 days post op, bought a couple of things and then walked home. Her CNS happened to phone her on her way back to see how she was, was delighted to hear she was out walking and said she might call on her to talk to women about bow to recover from a hysterectomy as many hardly move from the sofa for days. So walking is definitely good as long as you’re listening to your body.
You reminded me about something, in your post: I was a regular on Hyster Sisters when I had my surgery and recovery (many of those didn't have cancer, but had had a hysterectomy for other reasons) and the majority of them were the sofa ones...they were still sedentary or even in bed, three or four weeks after surgery!! Many also had taken the opportunity to get their partner to do the household chores!, so they weren't even lifting a finger to do washing up or similar. I live alone and always have done, so am used to being independent and doing everything for myself, so the motivation was there to get back to normal as quickly as was sensible!
Hi Dolly,
I had a total abdominal hysterectomy and bilateral salpingo oophorectomy a year ago. Was in hospital for four days but took walks up and down the ward every hour or so as soon as I was unhooked from various tubes and other paraphernalia. I’m 62 (61 at the time), lead an active lifestyle, otherwise fit and healthy and a stubborn old goat! I was therefore keen to push myself and walked every day as soon as I got home, gradually going a bit further and moving a bit faster every day.
I was told by hospital staff to listen to my body, which I thought at the time was a bit of a cop out, but it’s just so true! My body soon told me if it wasn’t happy and there were times when I overdid it, got bloated, sore and tired, and had to rein things right back in again.
Because mine was an open surgery, it was around 8 weeks before I felt comfortable driving as the seat belt sat right across my wound (I did go out for a run in the car to the garden centre with my husband around week 4 but put a cushion between my tum and the seatbelt).
The leaflet I got from the hospital advised starting pelvic floor exercises around 3 weeks post surgery and, yes, they’re for life! I’ve got into the habit of doing mine every morning in the shower and every night in bed before I put the light out, and I do notice a difference if I miss a few days.
At the end of the day there is no right nor wrong way to recover; only you know how you feel. Recovery can be frustrating but listen to your body and you’ll be back to normal in no time
Whatever cancer throws your way, we’re right there with you.
We’re here to provide physical, financial and emotional support.
© Macmillan Cancer Support 2026 © Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland. A company limited by guarantee, registered in England and Wales company number 2400969. Isle of Man company number 4694F. Registered office: 3rd Floor, Bronze Building, The Forge, 105 Sumner Street, London, SE1 9HZ. VAT no: 668265007