An Endoscopy is a procedure where the inside of your body is examined using an instrument called an endoscope. This is a long, thin, flexible tube that has a light source and camera at one end. Images of the inside of your body are relayed to a television screen. Endoscopes can be inserted into the body through a natural opening, such as the mouth and down the throat, or through the bottom. The mouth route is more accurately called a Gastroscopy and the anal route is called a Colonoscopy (or a reduced version called a Sigmoidoscopy). An endoscope can also be inserted through a small cut (incision) made in the skin when keyhole surgery is being carried out.
During a routine 6 monthly check-up at the end of 2016, I mentioned to my Oncologist that I was experiencing what appeared to be very minor heartburn and that it was an unusual symptom for me. He called forward my annual Echocardiogram and also ordered up a Gastroscopy.
I received the Gastroscopy paperwork from the hospital for an appointment on 26 Jan 2017. It offered an option for sedation, either a throat spray to numb the area or a sedative where I would probably not know what was going on. My initial thought was the latter even though it meant a longer visit to the hospital with some other constraints. It also meant I would need to check the sedation to assess the risk of NET Crisis. However, having discussed this issue with the department nurse, I was persuaded to go for the throat spray – apparently 80% of people opt for this method. I just couldn’t resist the statistical challenge! There were many advantages to selecting this option including getting rid of the sedation risk, plus I could walk out of the hospital immediately after the 5 minute procedure. The sedation option meant that I would need to remain in the hospital for an extra hour to recover, not drive for 24 hours and be supervised by an adult for 12 hours.
My blood pressure was checked prior to the procedure and systolic was around 145, 10-20 points above my normal ‘cool as a cucumber’ figure. Clearly, despite my deceptively stoic façade, something was making my heart work faster!
I was really put at ease by all 4 people in the room, two nurses, an endoscopic expert and a technician. However, the procedure itself is not what I would call a ‘breeze’. The throat spray was disgusting and said to taste of rotten bananas but personally I thought it was more like rotten fish! For the first 60 seconds (total guess) I found myself wishing I had gone for the sedation but the next minute was better after I had stopped ‘gagging’ and was now breathing fairly normally. I found swallowing easy despite the tube and a nurse was also extracting excess saliva using a similar tool used in a dental procedure. I was also aware that my eyes were watering! The natural reaction of ‘gagging’ came back at least once but only for a second or two. I would be lying if I said it wasn’t scary at the time.
The procedure seemed to be in parts, he checked the oesophagus, pumped air into my stomach for a better view, sprayed some water (not sure why), took a peek in the duodenum which required an extra swallow from me, using another tool, he took a painless routine sample from the stomach lining to test for CLO (Helicobacter Pylori – a bacterium in the lining of the stomach that can cause peptic ulcers), extracted the air, and then the extraction of the endoscope out from the gastrointestinal tract. These endoscopes really are like swiss army knives!
The best bit was the extraction! The other best bit was when he told me there were no real issues. So it was all worth it in the end! If anyone wants a copy of my comprehensive and easy to read 6 page Gastroscopy guide, let me know.
The other main type of Endoscopy is the Colonoscopy which enters the gastrointestinal tract in the opposite direction. I’ve had actually both a Gastroscopy and Colonoscopy before in 2008 before I was diagnosed. I offered the mandatory request to do the endoscopy first if using the same scope He’d heard it before! On this occasion I was fully sedated. One minute I was talking to the Gastroenterologist, then the next thing I remember was waking up, job done. Less stressful but more time intensive. That said, the preparation for the colonoscopy is no joke. You can read about this in my blog Colonoscopy Comedy which also includes a light-hearted story about the preparation phase. If you need a laugh, this is really funny.
Although I have not had these, for completeness, I want to mention several associated procedures.
For patients who have, or who are suspected of having pancreatic disease, their doctor may recommend that they undergo a type of procedure called an endoscopic ultrasound, or more often known as EUS. An EUS is a type of endoscopic examination. It involves the insertion of a thin tube into the mouth and down into the stomach and the first part of the small intestine. At the tip of the tube is a small ultrasound probe that emits sound waves. These sound waves bounce off of the surrounding structures, such as the stomach, small intestine, pancreas, bile ducts, and liver. These sound waves are then recaptured by the probe and converted into black and white images that are then interpreted by your doctor. Because the pancreas sits next to the stomach and small intestine, EUS allows the physician to get very detailed images of the pancreas. This procedure is typically performed in an outpatient setting, and usually takes between 20 and 45 minutes. One of the advantages of performing an EUS is that pancreatic biopsies can be obtained at the time of the examination. These biopsies, often referred to as FNA, or fine-needle aspiration, can allow for your physician to collect tissue samples which can later be analysed under a microscope. Special needles, designed to be used with the EUS scope, allow the physician to insert a small needle through the wall of the stomach or intestine directly into the pancreas. This video explains better: Click here.

“Camera Pill”
Shortly after I was diagnosed, this was mentioned as an option for me as my diagnostic scans were just showing a “mass” and it wasnt 100% clear where my primary tumour was located. It didn’t happen in the end. Capsule Endoscopy involves swallowing a small capsule (the size of the large vitamin pill). The ‘cam-pill’ contains a colour camera, battery, light source and transmitter. The camera takes two pictures every second for eight hours, transmitting images to a data recorder about the size of a portable CD player that patients wear around the waist.
Capsule endoscopy assists in diagnosing gastrointestinal conditions in the small bowel such as: bleeding, malabsorption, chronic abdominal pain, and chronic diarrhoea. Once swallowed the camera moves naturally through the digestive tract. Approximately eight hours after ingesting the camera, patients return to the Endoscopy Unit where the recording device is removed by the nurse, the images are downloaded to a computer and evaluated. The Capsule is disposable and will be passed naturally in the bowel movement.
 A flexible sigmoidoscopy is a procedure that is used to look inside the rectum (back passage) and lower part of your large bowel (descending colon) and so is like an abbreviated version of a colonoscopy.
A flexible sigmoidoscopy is a procedure that is used to look inside the rectum (back passage) and lower part of your large bowel (descending colon) and so is like an abbreviated version of a colonoscopy.
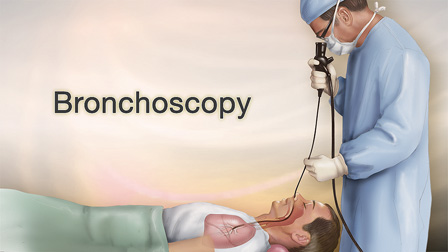 Bronchoscopy is a procedure that allows the doctor to examine your trachea (windpipe), bronchi (branches of the airway) and some areas of the lung. A short thin flexible tube with a mini camera built into its tip, called a ‘bronchoscope’, is used for this procedure. The bronchoscope is usually passed through your mouth or nose, into your trachea and bronchi. The doctor can then get a clear view of your airways. During the procedure, the doctor may take samples of tissue (biopsy) or respiratory secretions for examination. Bronchoscopies can also be used for ablation purposes. You may be interested in this award-winning biopsy and ablation service offered by the Royal Free Hospital in London UK – Innovation at Royal Free – Lung Biopsy and Radio Frequency Ablation Service
Bronchoscopy is a procedure that allows the doctor to examine your trachea (windpipe), bronchi (branches of the airway) and some areas of the lung. A short thin flexible tube with a mini camera built into its tip, called a ‘bronchoscope’, is used for this procedure. The bronchoscope is usually passed through your mouth or nose, into your trachea and bronchi. The doctor can then get a clear view of your airways. During the procedure, the doctor may take samples of tissue (biopsy) or respiratory secretions for examination. Bronchoscopies can also be used for ablation purposes. You may be interested in this award-winning biopsy and ablation service offered by the Royal Free Hospital in London UK – Innovation at Royal Free – Lung Biopsy and Radio Frequency Ablation Service
Thanks for reading about how physicians can take the camera directly to the sites of suspected tumours!
Ronny Allan
I’m also active on Facebook. Like my page for even more news.
Disclaimer
My Diagnosis and Treatment History
Most Popular Posts
Whatever cancer throws your way, we’re right there with you.
We’re here to provide physical, financial and emotional support.
© Macmillan Cancer Support 2024 © Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland. A company limited by guarantee, registered in England and Wales company number 2400969. Isle of Man company number 4694F. Registered office: 3rd Floor, Bronze Building, The Forge, 105 Sumner Street, London, SE1 9HZ. VAT no: 668265007