April is testicular cancer awareness month. Around 2,400 men are diagnosed with testicular cancer each year in the UK[1].
That’s more than 6 a day!
Testicular cancer can affect anyone who has testicles including men, trans women and people assigned male at birth. It is more likely to happen between the ages of 25-40 but can happen at any age.
Testicular cancer is usually curable. Being aware of symptoms, how to check for them, and seeing your GP sooner rather than later can help find testicular cancer earlier when it is easier to treat.
What is testicular cancer?
Testicular cancer starts in one of the testicles. The testicles are 2 oval-shaped organs inside the scrotum. The scrotum is a pouch of skin behind the penis. The testicles hang below the penis. They are sometimes called the testes. The testicles are the main part of the male reproductive system.
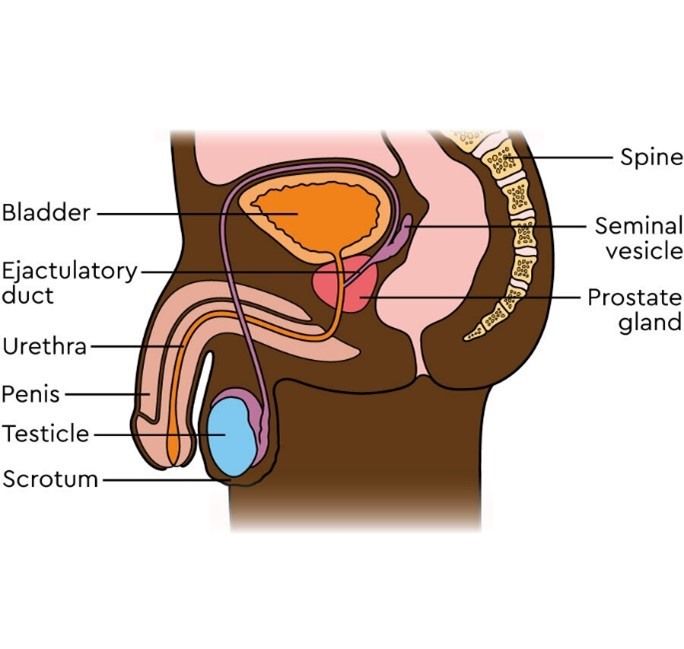
Testicular cancer is usually only found in the testicle, but sometimes cancer cells from the testicles can spread to nearby lymph nodes.
Are there any causes or risk factors?
Doctors do not yet know what causes testicular cancer. But we know some of the risk factors that may increase the chances of developing it. These include:
CIS is sometimes found after having a biopsy of the testicle – for example, to investigate infertility (being unable to start a pregnancy).
Factors that do not increase risk
There is no evidence to suggest that injury to a testicle increases your risk of getting testicular cancer. But an injury to a testicle or the groin may bring possible symptoms of testicular cancer to your doctor’s attention. Having a vasectomy does not increase the risk of getting testicular cancer.
What are the symptoms of testicular cancer?
The main symptom of testicular cancer is a lump in the testicle. Some people also have other symptoms. These include:
If the cancer has spread to lymph nodes or other parts of the body, it may cause other symptoms such as
Conditions other than testicular cancer may cause these signs and symptoms. It is always important to get your symptoms checked by your doctor.
How do I check for testicular cancer?
From puberty onwards, it is important to check your testicles regularly, for example, every month. Doing regularly checks means you will soon get to know what feels normal for you.
A normal testicle should feel smooth and firm, but not hard.
It can be easier to check your testicles during, or right after, a warm bath or shower when the scrotal skin is relaxed.
Hold your scrotum in the palm of your hand. Use your fingers and thumb to examine each testicle. You should feel for:
It is normal for the testicles to be slightly different in size. It is also normal for one to hang lower than the other.
Orchid have a fantastic leaflet you can download which contains lots of helpful information about signs and symptoms and Testicular Self-Examination (TSE).
If I’m worried, what should I do?
It is important to get your GP to check anything unusual as soon as possible. You could also visit your local sexual health clinic. You can find your nearest clinic on the NHS website.
It might feel embarrassing talking to your GP, but they are used to dealing with problems like this. And they are there to support you.
Support if you are LGBTQ+
If you are a trans woman and have testicles, you may feel uncomfortable or upset about checking this part of the body. It is still important to get any changes checked. There is additional support available, such as talking to a gender identity clinic or a sexual health service that is trans and non-binary friendly. You can check if this is available in your area on Tranzwiki.
What happens when I see my GP?
Your GP will examine you. If they think your symptoms may be linked to testicular cancer, they will refer you to a hospital to be seen within 2 weeks. Sometimes, your GP will arrange for an ultrasound scan of the testicle before you visit the hospital.
Tests and treatment
At the hospital, you will see a urologist. This is a doctor who specialises in treating problems with the testicles, penis, prostate, bladder and kidneys. They will:
Some hospitals have testicular one-stop clinics. This means as well as seeing a urology doctor, you may have an ultrasound on the same day. You will also be seen by a specialist nurse.
If the ultrasound shows the lump is highly likely to be testicular cancer, the whole testicle needs to be closely examined.
The only way to confirm a diagnosis is to remove the affected testicle by surgery (orchidectomy). This also removes the cancer and is the main treatment for testicular cancer that has not spread. If the other testicle is healthy, an orchidectomy will not affect your ability to get an erection or your fertility. Your doctor or nurse can explain more about this.
Surgery may be the only treatment you will need.
After this your doctors and team of specialists may talk to you about the treatment options. They will explain what might be best in your situation. Treatment options depend on:
They may talk to you about surveillance. This is the option of monitoring you regularly in clinic. Or they may suggest having chemotherapy after surgery. Occasionally, they may suggest radiotherapy.
So remember, regular checks + early detection + getting seen early = big difference
The ball is in your court!
If you are worried about testicular cancer and would like to talk to someone, we’re here. You can
Further Information and support
Read
Understanding testicular cancer booklet
How to check your ball (testicles) easy read
Online
Macmillan website – testicular cancer
Online forums
The online community has lots of blogs and forums where people can write about their own personal experiences and share their stories.
Online Forum (testicular cancer)
Orchid is the UK’s leading charity for those affected by male cancer, including testicular cancer. They off a wide range of support services to males of all ages including a freephone National Male Cancer helpline.
Watch
Video: Let’s talk balls with Justin and Matt
Listen
What matters to me podcast – Episode 3 : Matt’s story. Matt shares his story of being diagnosed with testicular cancer and how Macmillan support helped him when his diagnosis affected his mental health.
References
[1] https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/testicular-cancer
Whatever cancer throws your way, we’re right there with you.
We’re here to provide physical, financial and emotional support.
© Macmillan Cancer Support 2026 © Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland. A company limited by guarantee, registered in England and Wales company number 2400969. Isle of Man company number 4694F. Registered office: 3rd Floor, Bronze Building, The Forge, 105 Sumner Street, London, SE1 9HZ. VAT no: 668265007