[originally published on 14 October 2023]
Introduction
When I put together some brief reflections on Preston recently, having moved out of the city last month, I half expected my next post to be about a new ‘cracking’ adventure. Aside from returning home to North Norfolk, I knew that I would soon be applying for new roles. I did not know where I would be living and working, or whether that adventure would be an extended trip abroad or some other kind of challenge. I began to feel that excitement once more of not knowing. However, I recently received some distressing news about my physical health, which I had only alluded to in that previous post, without naming it. I had partly mentally prepared myself for the news, but was still somewhat shocked when I found out. It will, therefore, be some other kind of challenge that I was not really expecting just one month ago. Up until now I have kept this information private, telling close family and friends only, but I’m going public because there is still a tendency, especially amongst men, to ignore or dismiss physical health symptoms. It is also getting tiring repeating my story to one person at a time. If you are interested to know more, then please read on. But please note that it contains lots of personal and intimate details.
The story so far..
Back on 18 May, excited by a new version of my infamous EAP parody* almost being completed, I went out with work colleagues for a drunken evening that went on a bit longer than my body probably needed. I smoked cigarettes, which I don’t usually do. I was unsurprisingly hungover the following day and my anxiety returned over the subsequent days. On 22 May, I ‘crashed’ at work again, overwhelmed with catastrophising thoughts and it wasn’t long before I was signed off sick again. I missed my final CBT booster session and returned to North Norfolk for a week with family. I wasn’t well – mentally anyway. I couldn’t work out why this was happening yet again. It didn’t help much as I was just worried the whole week about returning to work. However, I did manage to record my fastest parkrun time to date at Holkham. Physically, I did notice some minor constipation at this time, but that was all.
During June, while ‘signed off’, I failed to attend both the department’s annual conference as well as the Therapy Summit organised by the Social Prescribing Unit with Mind Over Mountains – something I had been really looking forward to. I got cold feet on the day and turned around at the bus station, unable to face people. I crawled back home and went back to bed. July was worse. Most physical activity, which I wrote about earlier this year, had declined in June and this plummeted in July as some wet weather hit the Lancashire region. It was unusual to be like this during the summer, when I am normally up and about doing things outside. I declined further and my physical problems began to increasingly bother me. I felt alone. The constipation continued, but now there was also some bleeding when going to the toilet. I would usually feel bloated and this led to frequent toileting, never wanting to be more than 10 minutes away from a loo. I began to eat and exercise less. I think I was mildly depressed, too. This merely exacerbated the problem. For a couple of weeks I tried to treat it myself, including trying over the counter products such as FyboCalm, Milk of Magnesia, applying Anusol for possible haemorrhoids and even drinking Brandy to try to aid digestion. In addition, I often thought of Hermione Granger’s advice around ‘Devil’s Snare’ when going to the toilet. You can’t fight it or force it! None of this really worked, although the cream probably kept things calm – at least externally. Finally, on the day that the much respected BBC newsreader, George Alagiah (below), died of bowel cancer (24 July) having first been diagnosed in 2014, I contacted my GP surgery. I finally had an appointment a few days later (27 July), roughly four weeks after I first had the thought to ring them. Typical man, eh? I sort of dismissed the symptoms, thought they would simply pass or could be self treated.
On the recommendation of a GP, I undertook a Faecal Immunochemical Test, providing two stool samples to my surgery the next day. I was prescribed CosmoCol laxative and some bloods were taken, too. The laxative worked but I had to stop as things went too far the other way. Nonetheless, it was sufficient to provide the required samples and a few days later the FIT came back positive. I was immediately referred to the Lower Gastrointestinal (GI) team at Preston hospital. Some bloods were consequently taken, too. The bloods revealed that I had ‘slight Iron-deficiency anaemia’ according to a text from the doctor who saw me, although I later found out my levels (around a ‘5’) were more than ‘slight’. On 14 August, I was prescribed some heavy duty Ferrous Fumarate capsules, without any consultation. With a prime side effect being constipation, I was reluctant to take them and looked for more natural ways to ingest iron – for example Kale and Spirulina. Also worryingly, when I weighed myself for the first time in months, I had somehow lost 8kg (17lbs) between March and August after being a consistent weight for years. Some ‘before’ and ‘after’ photographic evidence seemed to confirm this. You can probably work out where this story is now going..
Around this time, work contacted me and called a meeting about my prolonged absence. Only during the first of two ‘incapacity procedure’ meetings did I finally reveal my physical ailments. I reflected on the amount of ‘sick leave’ accrued, not knowing how I would be ‘accommodated’ again, and without a proper diagnosis for my physical condition, I decided to quit and give just under one months notice, which was accepted in the circumstances. At the same time I gave one month’s notice on my rented flat. When a great family friend and former tenant died suddenly on 22 August and there was news of another friend’s sudden death back home in July, I felt a real urge to be back with family. It was stressful packing, cleaning and leaving my flat in an excellent condition. However, in hindsight, it was definitely the right decision to leave both my fantastic job and Preston after two years.
Endoscopy and Colonoscopy
As a consequence of my lower GI referral and a telephone call from the GI team two weeks prior, on 20 September, I returned to Preston. I spent an uncomfortable night in an empty house in Garstang – which had been vacated that day by my Australian friend and former work colleague. I did not eat for 26 hours. Whilst there, I took or tried to consume two litres of another, stronger laxative, MoviPrep, with water. This was a challenge. My stomach quickly became full and I threw up around 20% of what I swallowed. I had cleared my bowels to about 80% – not ideal, but enough. The next day I attended an InHealth mobile Endoscopy unit. I had been referred there on 6 September by the department of Colorectal Surgery at Royal Preston Hospital, Fulwood. Under the ‘two week rule’, due to having frequent blood loss from my rectum, a positive faecal occult blood result and iron deficient anaemia, this was an urgent referral. As well as undergoing a transnasal endoscopy, I also underwent a full colonoscopy for the first time in my life. A Xylocaine Spray was delivered to my nose, which the scope was sent up, and throat, thereby passing my potentially strong gag reflex. The scope was retroflexed into the stomach with the procedure completed successfully. Several samples of my stomach were taken for a biopsy. At the same appointment, I was turned around and a different scope was used to enter my rectum. This created more discomfort than the endoscopy and was painful at times. I only took gas and air, no further sedative, despite having a canular in my arm. I got through this, but the doctor could not get beyond a blockage in my lower colon. The procedure was aborted as the room went quiet, notes were made and I was wheeled into the recovery room, where I quickly consumed two cups of tea and several, tasty biscuits. The doctor who performed both procedures arrived to announce that the endoscopy revealed that I had non-erosive gastritis (inflammation) and was recommended to take Omeprazole. This is easily treatable with medication, diet (such as non-spicy foods), not consuming alcohol and ‘grounding’! According to Oschman, J. L., Chevalier, G., & Brown, R (2015), multi-disciplinary research has revealed that electrically conductive contact of the human body with the surface of the Earth (grounding or earthing) produces intriguing effects on physiology and health … including reducing inflammation. However, the more concerning finding was a growth (or tumour) found in my large colon. It would likely require surgery to remove it, but first the biopsies would show if there was anything cancerous. So I had to wait.
How common is bowel cancer?
Bowel cancer is the fourth most common cancer in the UK. Almost 43,000 people are diagnosed with bowel cancer every year in the UK. Around 268,000 people living in the UK today have been diagnosed with bowel cancer. More than nine out of ten new cases (94%) are diagnosed in people over the age of 50. But bowel cancer can affect anyone of any age. More than 2,600 new cases are diagnosed in people under the age of 50 every year. 1 in 15 men and 1 in 18 women will be diagnosed with bowel cancer during their lifetime.
[source: Bowel Cancer UK]
Diagnosis and Description
One week later, I returned for further blood tests, at my request, to check my anaemia level and to have a CT scan. It could have been sooner, but I wanted to attend a pre-arranged job interview in Greenwich on 28 September. I didn’t get the job, despite a great presentation, and found visiting London quite stressful. The CT scan on 29 September went smoothly, but I continued to struggle with discomfort in different parts of my body. I began noticing something further up – not in my digestive system but something else on the right-hand side. Another week went by. I allowed for the NHS strikes (including consultants) that occurred during this week, and then chased the biopsy results.
On Wednesday 4 October, the news came that I had begun to fear. I was informed by a member of the Multidisciplinary Team (MDT) in Preston that I had T3 tumour carrying cancer cells in my bowel. The bowel wall is made up of layers of different tissues. Under the TNM staging system, the ones in bold apply to me:
T – describes how far the tumour has grown into the wall of the bowel, and whether it has grown into nearby tissues or organs.
N – describes whether the cancer has spread to the lymph nodes.
M – describes whether the cancer has spread to another part of the body such as the liver or lungs (secondary or metastatic cancer).
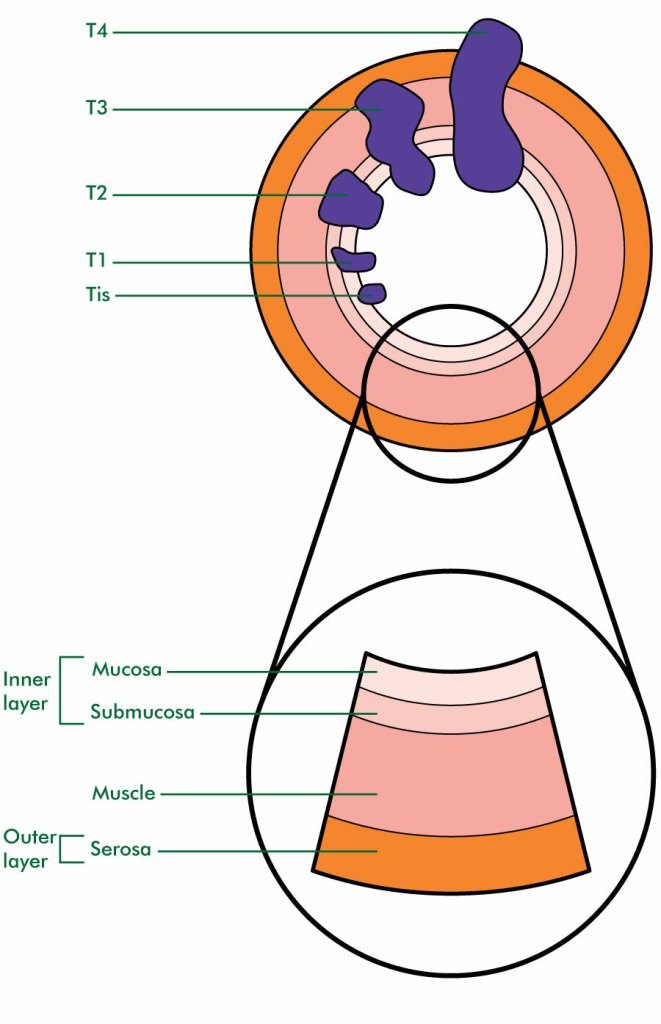
In addition, according to the staging system, I had N2 infection of some lymph nodes, although until a further scan I do not know how many are currently affected. Again this is broken down as such:
N0 means no lymph nodes contain cancer cells.
N1 means there are cancer cells in up to three nearby lymph nodes or there are cancer cells in the tissues around the bowel. N1 is split into 3 stages – N1a, N1b and N1c:
N2 means there are cancer cells in four or more nearby lymph nodes. N2 is split into 2 stages – N2a and N2b:
Furthermore, the CT scan had initially showed a potential abnormality in my liver, which made sense given that I had felt something in that area. If the original cancer spreads, this is known as metastases (or ‘mets’). M0 means the cancer has not spread to distant organs. However, M1 means the cancer has spread to distant organs such as the liver or lungs. At this point the overall stage is described as 4! I probably have M1a as described below.
There are 2 stages of cancer spread (metastasis):
M0 means the cancer has not spread to other organs.
M1 means the cancer has spread to other parts of the body such as the lung or liver. Again, I need further scans to determine the exact nature of this worrying spread. There are 3 stages here: M1a, M1b and M1c:
• M1a means the cancer has spread to 1 distant site or organ, for example the liver, but it hasn’t spread to the tissue lining your tummy (peritoneum)
• M1b means the cancer has spread to 2 or more distant sites or organs, but it hasn’t spread to the tissue lining your peritoneum
• M1c means the cancer may have spread to distant organs and it has spread to your peritoneum
My lungs – which are higher up – are fine, so I don’t feel guilty about any cigarettes I might have had on 22 May. But the liver news is worrying. Subsequently, I was advised that an MRI or PET-CT scan would be needed to determine whether the liver had been infected and whether any growth there was malignant or benign. Again, it could mean potential surgery. After a few phone calls it was agreed that returning to Preston yet again would be unnecessary and a Teams meeting was set up to discuss the findings so far.
The Consultation Clinic
I did not wish to return for a third time to Preston – it is a 440 mile round trip after all – but would have done so if it meant the further scans could be carried out sooner rather than later. Instead, on 10 October (coinciding with World Mental Health Day), I had a video consultation, on Teams, with the doctor responsible for informing me of all the findings so far and the prognosis going forward. As well as confirming the T3 bowel cancer, he also confirmed there are three separate abnormalities on the liver. A large 6.8cm (golf ball size) growth on the left-hand side and two smaller (1.8cm and 1.2cm) growths on the right-hand side. This meant that they have to proceed using a systemic approach to treatment. Liver surgery could be option in the future. For now, though, I would probably need to have minor surgery – a stoma (with colostomy bag) fitted. This would be followed by a course of chemotherapy which will probably run for months. Meanwhile, everything would be transferred from Preston to the relevant oncology unit at Norfolk & Norwich hospital. I have already re-registered at my local GP surgery and requested copies of all the findings so far. My immediate family were told my diagnosis and prognosis on this day. In addition, I contacted a couple of friends, too. Which brings me onto the emotional aspect of all of this.
Feelings
According to Bowel Cancer UK the diagnosed patient and loved ones are all likely to feel a range of emotions. I actually took the news calmly and have remained relatively calm ever since. I began to worry more as my symptoms have persisted. For someone prone to panic, I have so far not done so. Nonetheless, I was shocked to discover how advanced the cancer is. The anxiety that I was going through earlier this year might have exacerbated the symptoms, though. However, not knowing is the worst thing of all. Being given timely and accurate information is crucial. Waiting for an appointment or a telephone call can be frustrating, so I am learning to be a patient patient. I can be irritable at times, but then I have got cause to complain a bit now. I can see myself getting more irritable, too. For months I was looking for cushions to sit on every time I went out, but not everyone had the patience to listen to my list of ailments. It is good to ask someone how they feel about their diagnosis. Other experiences can be useful, but only if it adds to the sum of knowledge. This clearly affects people in different ways, so it is not always appropriate to give the best or worst case scenario! I never would have believed, not least when I was park running, going to the gym and eating healthily at the beginning of this year, that at the age of 52 I would be needing a colostomy bag and chemotherapy by the end of it! I am still processing this revelation, but writing this diary is therapeutic.
Reflection
My extensive experience of tutoring student nurses at UCLan has put me in a good place to understand the terminology used so far, procedures being followed and the pressures that NHS staff are under. I advised many students over the past two years on their reflective essays, often using Gibbs’ Reflective Cycle (shown above), which they needed to complete in each year of their undergraduate studies. I mentioned this fact to the MDT representative on 10 October. Whilst I am not using this model exactly to frame my own reflection on this new journey, I will continue to describe what is happening, write about my feelings, evaluating the process and any action that is taken. I have called this entry ‘Part 1’ as there will definitely be a ‘Part 2’. Given the seriousness and advanced stage of my cancer, it is likely there will be more as I chronicle my new, unexpected journey. Of course, with any cancer you never know the future or what I will have to face in the coming months. But I am prepared and will conclude by justifying this post.
“Oh, there’s so much to live for
So much lеft to give
This edition is limited
Thеre’s only so much can be done”
Conclusion
As I stated at the beginning, I have published this diary for anyone to see, but I did consider whether to do so or not. There are two main reasons, with a third reason, which I will finish off by mentioning. The first reason is that having individually told family and close friends, I was beginning to find it tiring going through it all again. The second reason I have done so is because there is still a tendency, especially amongst men, to ignore or dismiss symptoms. I am guilty of this to some degree and self treatment was not the answer. All the signs were there, but I was a bit slow to respond. Just this week, TV sports presenter, Steve Rider revealed he had a prostate cancer diagnosis but it had been caught early. The 73 year-old has gone from initial concerns to a diagnosis and onto an operation in 2 months. He said exactly the same thing on BBC Breakfast on 11 October about catching these things early.. leave it six months and it is more problematic.
Hindsight is a wonderful thing, of course, and I could have contacted my GP surgery sooner. But it is what it is. At present, I have only minor regrets on the timing of it all. Anyone that knows me, knows that I have resilience and have proven this many times in my life. It will not stop me from applying for jobs and going to interviews as, with modern advances in medicine, people can make full recoveries from treatment. However, it might be a while before I can realistically be in full-time employment again. I am facing this head on and will maintain a positive attitude throughout, and I know there is plenty of support out there! With help, I intend to kick this cancer’s arse!! Which is what I have called this new blog!!
Despite all my symptoms indicating possible bowel cancer, it was not until I picked up an information leaflet at the hospital on 21 September, that I felt that I probably had it. Although I suspected something was (seriously) wrong, just as I did when I got Malaria in Tanzania and Covid-19 last year, I did not want to talk up the possibility and never discussed this thought with friends or family until after my two procedures on that date – even though behind the scenes things were being said. My suspicions had already been raised before the diagnosis and in mid-September I saw that my good friend, Meriol, was doing Sober October. So I was inspired to sign up, too, knowing that my diagnosis might reveal an additional reason to fundraise this time around, having raised some funds during ‘cold water’ July last year. Given my diagnosis it makes sense to stay off the booze! Drinking alcohol is not good for the liver. Consuming a large quantity of it puts pressure on the liver, as it needs to work harder to process it all. The liver can get exhausted. It can regenerate itself, but needs to be given a chance. It produces new cells with the intention to fix problems. It is important to stay in good shape and limit alcohol intake for this reason.
I am already reading articles on Macmillan’s support pages on a daily basis and will soon be accessing their forums. If you leave a supportive comment on this blog post, I will be very grateful.
Thank you for reading all the way to the end!
Note: Product (brand) names have been deliberately written in italics.
*The EAP parody, ‘Paraphase (2023)’ was eventually completed, but removed from YouTube after a few days at the request of the university marketing department.
References:
Bowel Cancer UK (2023). About Bowel Cancer. Available at: https://www.bowelcanceruk.org.uk/about-bowel-cancer/bowel-cancer/. Accessed 10 October 2023.
Bowel Cancer UK (2023). Symptoms of Bowel Cancer. Available at: https://www.bowelcanceruk.org.uk/about-bowel-cancer/symptoms/. Accessed 4 October 2023.
Bowel Cancer UK (2023). Supporting someone with bowel cancer. Available at: https://www.bowelcanceruk.org.uk/about-bowel-cancer/living-with-and-beyond-bowel-cancer/emotional-wellbeing/supporting-someone-with-bowel-cancer. Accessed 8 October 2023.
Cancer Research UK (2023). TNM Staging. Available at: https://www.cancerresearchuk.org/about-cancer/bowel-cancer/stages-types-and-grades/TNM-staging. Accessed 9 October 2023.
Macmillan Cancer Support (2023). Bowel cancer and lymph nodes. Available at: https://www.macmillan.org.uk/cancer-information-and-support/bowel-cancer/bowel-cancer-and-the-lymphatic-system. Accessed 4 October 2023.
Macmillan Cancer Support (2023). Staging and grading of bowel cancer. Available at: https://www.macmillan.org.uk/cancer-information-and-support/bowel-cancer/staging-and-grading-of-bowel-cancer. Accessed 4 October 2023.
Macmillan Cancer Support (2023). What Your Body Does After One Month off Alcohol. Available at: https://www.gosober.org.uk/blogs/wellbeing/what-your-body-does-after-one-month-off-alcohol/. Accessed 10 October 2023.
Mills, K-A. (2023). Three Keys Signs of Bowel Cancer You Need to Know – from blood to weight loss. Available at: https://www.msn.com/en-gb/health/medical/three-key-signs-of-bowel-cancer-you-need-to-know-from-blood-to-weight-loss/. Accessed 9 October 2023.
Mind Tools Ltd (2023). Gibbs’ Reflective Cycle. Available at: https://www.mindtools.com/ano9qiu/gibbs-reflective-cycle. Accessed 7 October 2023.
Oschman, J. L., Chevalier, G., & Brown, R. (2015). The effects of grounding (earthing) on inflammation, the immune response, wound healing, and prevention and treatment of chronic inflammatory and autoimmune diseases. Journal of inflammation research, 8, 83–96. https://doi.org/10.2147/JIR.S69656. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378297/. Accessed on 8 October 2023.
Whatever cancer throws your way, we’re right there with you.
We’re here to provide physical, financial and emotional support.
© Macmillan Cancer Support 2026 © Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland. A company limited by guarantee, registered in England and Wales company number 2400969. Isle of Man company number 4694F. Registered office: 3rd Floor, Bronze Building, The Forge, 105 Sumner Street, London, SE1 9HZ. VAT no: 668265007