Introduction
This is the second part of my cancer diary, which details the past month. The first part of my cancer diary was published on this WordPress blog on the evening of 14 October. Over the course of that evening and the next day alone, my blog received 220 unique visitors and 684 views. This is the most ever in the first 48 hours of publishing a new post! Visitors naturally dropped off the following week, but it clearly resonated with people. It has encouraged me to continue to publicise what would otherwise be a very private diary. I received a lot of ‘public’ messages on my blog, Facebook, my private, non -professional Instagram account and the more professional LinkedIn, where I shared my post on 16 October. As I stated on there, I shared it because some people told me that my writing is not only personalised, but also educational and the first part in particular might even help to save a life. In addition, many people sent me ‘private’ (direct) messages – one way or another – and I always respond to those. I haven’t been so overwhelmed about a post since I put the request out for my original mental health in ELT survey in December 2017. It is tiring to provide a running commentary, giving updates, so it is easier for me to collect my thoughts into a monthly diary such as this and share that. For family and close friends, of course, I will always answer questions as they have a more practical role in supporting me. All support is welcome though. As with part one, continue to read if you want to, but please note that this second post contains lots of personal and intimate details.
Full Diagnosis
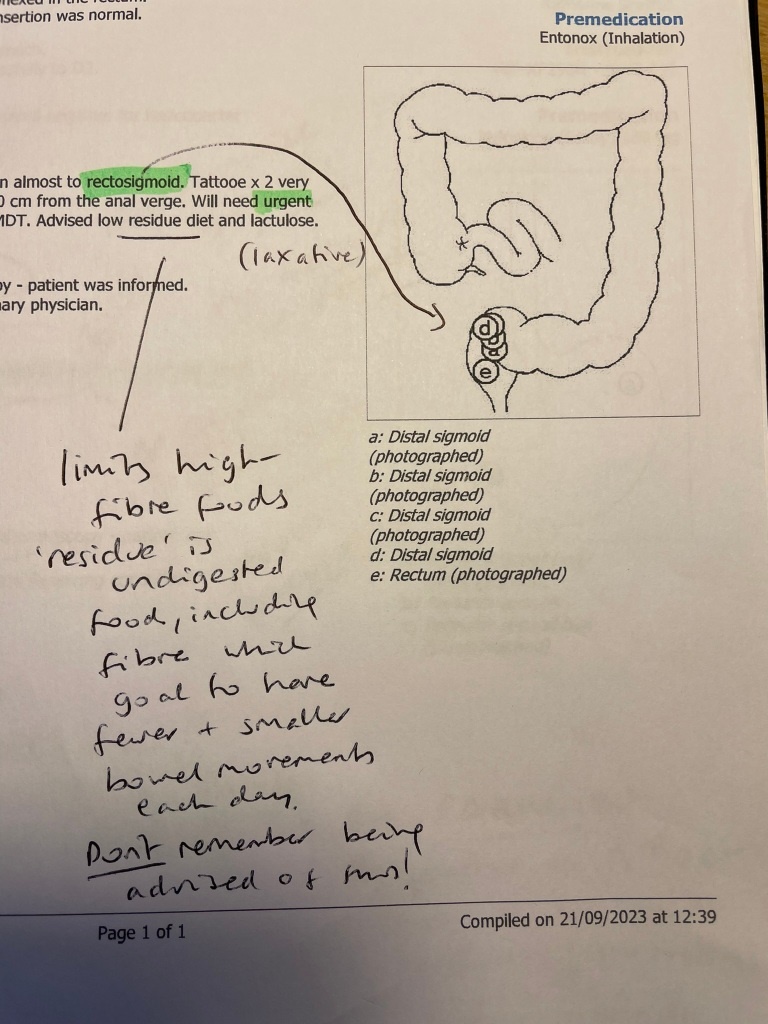
When the endoscopy and colonoscopy was carried out in Preston on 21 September, I was given a report of the former, but not the latter. It was an oversight. I chased it a couple of times until, at the third time of asking, on 23 October, I was finally sent the one-page report by email, showing a crude diagram of where the cancerous tumour was in my bowel. The tumour appeared to be further down the sigmoid (lower, horizontal part), and closer to my rectum than first thought – actually described as ‘an impassable distal sigmoid almost to rectosigmoid’. A few days later, on 27 October, I finally received a copy of some letters, dated 11 October, that had been sent to my GP surgery in North Norfolk and the Colorectal Cancer Multi Disciplinary Team (MDT) at the Norfolk and Norwich University hospital (NNUH). The latter was excellent, very detailed and restated that I had rectosigmoid cancer with multiple liver metastases. It also stated the histology confirmed ‘moderately differentiated adenocarcinoma with proficient MMR (Mismatch Repair)’ and the urgency of treatment. Like many bowel cancers, it is fortunately slow growing (grade 2, see below), giving me a bit of time, but still in urgent need of a stoma operation, as if this original tumour grew any more I would not have been able to go to toilet at all, which I go into more detail below.
The grades of bowel cancer cells are from 1 to 4:
Low grade – slow growing
High grade – fast growing
Adenocarcinoma, which is the first time I have heard of this, is a type of cancer that starts in the glands that line the insides of the organs, so it can affect different body areas. Adenocarcinoma forms in glandular epithelial cells, which secrete mucus, digestive juices or other fluids. In some cases, adenocarcinoma spreads to other parts of the body and, at that point, it is called metastatic adenocarcinoma. In bowel cancer, it starts in the gland cells in the lining of the bowel wall. The mucus produced is a slimy substance that makes it easier for faeces (poo) to pass through the bowel. Adenocarcinoma is the most common type of bowel cancer. So, whilst I might never know when this started, it is likely that it started in this way – possibly in May, maybe earlier (information adapted from Cancer Research UK, 2023).
Furthermore, the detailed letter to the Norwich MDT confirmed the T3a N2 M1a staging that I had worked out from previous consultations and stated in my previous post. ‘Several’ hepatic (liver) metastases including a large lesion in the left hepatic lobe measuring 6.8cm meant that a MR liver scan and/or a PET scan is also recommended, as well as a defunctioning colostomy operation and systemic chemotherapy after that. The scan(s) would occur between the two.
Low Residue Diet

The colonoscopy report also stated that I was advised to go onto a low residue (low fibre/roughage) diet. I tried to keep to this before the two September procedures, but I should have carried on afterwards and continued with this, especially with an operation coming up. After that, I should be able to return to a relatively ‘normal’ diet. For years, I have had a high fibre diet by choice, preferring all the foods on the right-hand side of the list below, compared to the left-hand side. But a good friend and holistic coach in Preston earlier this year pointed out that you can have too much fibre – and, indeed, if you do, you might develop blockages from undigested food in the bowel. Avoid fat, too much sugar and raw salad and vegetables. If you are going to have veg, then cook it well or use a juicer. Overcooking might remove some of the nutritious content, but it makes it more digestible. Despite being counter intuitive, I was prepared to follow the guidance. The first meal I created at home was a chicken and mushroom risotto, with well-cooked vegetables and parmesan (see below).
I also sought other forms of food and drink to consume. One recommendation was to regularly consume watermelon and Aloe Vera juice drink. I invested before I digested. This low residue dietary requirement was taken seriously. It is believed that all melons have ‘healing’ properties. They are one of the most hydrating foods you can eat. They are predigested—meaning that melon flesh is so assimilable that our digestive systems barely need to process it when it enters the body, because it is so high in enzymes. The fructose in melon leaves the stomach in less than one minute, then the rest of the fruit drops directly into the intestinal tract, immediately fortifying and replenishing the body. Eating well and appropriately goes some way to alleviate any fears I might have about self treatment.
Fear and Coping
You might wonder how I am coping with all of this so far? Well, my extensive history of anxiety and so-called ‘panic attacks’ has taught me that any anxiety I am going through now will pass or can be managed. The book by Joshua Fletcher and Dean Stott that I recommended earlier this year taught me a lot about how to react to ‘fear’ and stressors. I am not going to take this lying down (apart from immediately after an operation) and have been staying physically active by walking around town every day and running on Saturdays. A cancer diagnosis can be scary, but I am determined to keep active and even have a bit of fun, such as running around Holkham in a borrowed ‘Scream’ mask on 28 October! Probably my last parkrun for a while, although I might walk the next time. Just going up flights of stairs several times a day helps, too. My resting heart rate is usually around 60-65bpm. I constantly monitor my body battery and sleep, with the Garmin smart watch I was given for my 52nd birthday this year, along with the associated app on my mobile phone. In hospital blood pressure is, of course, constantly monitored, amongst many other indicators of vital signs.
The main thing that bothers me is the waiting to be seen and for receiving timely information and advice. So far, I have not felt bitter at all. I certainly don’t wonder why the hell it is happening to me, but acceptance happens in stages. Uncertainty can be hard to deal with. It can make you feel anxious, angry, irritable and frightened. This can impact on family members around you, especially when they are also struggling with their own health concerns. I am very keen to know everything and don’t shy away from worst-case scenarios. Other people do seem more worried than I am. However, I know that roughly 1 in 2 people will have a cancer diagnosis in their lifetime, so I remain positive and believe that with the right treatment I will be able to beat this. But it is a marathon, not a sprint!
Stoma Education
Another good friend, Sandy, recommended this excellent resource from Crohn’s & Colitis UK about living with a stoma in a comment on my first post. It answered a lot of questions that I had already formed. If you have a stoma (Greek for ‘mouth’), you’re not alone. Around 190,000 people in the UK have a stoma. Furthermore, on 24 October, I had a Zoom chat with another Anglia [Polytechnic/Ruskin] University graduate, from the class of 2001, and her partner about living with a stoma. He had been doing so for 30 years, so this was welcome and a positive take which allayed some fears I had. His was an ileostomy, rather than a colostomy – which is what I was going to have. An ileostomy is made from a part of your small bowel called the ileum. A colostomy is made from a part of your large bowel or colon – which is where my problem resides. This 30 minute chat helped to shift my perception from reluctant to more welcoming. It was just the reassurance I needed ahead of my operation.
According to the above website, if you have surgery to remove part of your bowel, the joined ends of the bowel can be delicate and leaky at first. Or sometimes it might not be appropriate to join the bowel straightaway. A temporary stoma keeps the contents of your gut away from the delicate sections of bowel. This gives your bowel time to heal. Once it’s healed, you can have more surgery to remove the stoma. This is usually months or sometimes years later. Depending on the type of surgery you’ve had, you might need more than one operation to reverse the stoma. After stoma reversal, you usually have a scar 1 to 2cm longer than the stoma, but these days laparoscopic surgery is actually less invasive. Some people decide they do not want to have the stoma reversed as they become used to it. Sometimes, it cannot be reversed at all. My own operation is described further down.
A Sober Estimate

Sober October ended on 31 October, with £230* raised for Macmillan. On 1 November, I had some red wine, my first alcoholic drink since I struggled to down two Belgian beers in a pub in Preston on 30 September, my last day in the city. I believe it is the first full month I have gone without alcohol since I was living in Riyadh, 2011. Even then I had lots of non-alcoholic lager. Prior to that, the only time I can recall going more than a month without was probably when I contracted campylobacter whilst a student at Anglia University in Cambridge, 2000. That remains the most unwell I have ever been; worse than contracting malaria in Tanzania several years later. I’ve worked in a Real Ale Shop and in a bar and restaurant in Wells-next-the-Sea, so have often been around or drinking booze. I might have been sober for a month or longer at other times, but I don’t remember when.
It is obviously good to give your body a rest – which is why ‘Dry January’ is so popular. The health benefits are widely known, not least the rest it gives the liver. I’m also very clear-headed now, seemingly able to remember and retain more information than before. Regardless of the fundraising, I would have had a month off anyway, given my gastritis and liver mets. Drinking might have even been one of the causes of developing an adenocarcinoma in the first place – but that will be very difficult to establish or when exactly it starting to develop. But I suspect my moderate drinking in August and early September did not help. When the chemotherapy comes around, I will probably have to stop again, so it is looking like a sober Christmas and New Year for me – although I might make an exception on Christmas Day and New Year’s Eve. My mother has a biblical phrase (Romans 12:3) that is about not getting ahead of yourself or thinking too highly of ourselves. We should, instead, ‘consider ourselves with sober judgement’. So taking a sober estimate of any situation means not getting carried away – and, in my case, not getting arrogant – one of my worst, occasional traits.
MDT Decision
On 1 November, as my sober month ended, I was rung by a colorectal nurse about what would happen next. Initially, I was phoned immediately following the long-awaited Multidisciplinary team (MDT) meeting. To my mild relief, they had provisionally arranged my stoma (defunctioning colostomy) operation for 21 November. Given that I had a scheduled meeting with the stoma doctor (surgeon) on 15 November, that seemed reasonable. A referral for a PET-CT or MRI scan of my liver was also arranged, as well as the oncology department being informed about the need for systemic chemotherapy. The urgency of the wording in the Royal Preston letters appeared to have pushed things through quite quickly. I felt good that after weeks of waiting, some (ahem) movement was finally happening on this. However, 3 weeks still seemed a long way off.
Then, later that day, with some ‘alarm bells’ ringing, I was phoned again to be informed that the doctor who was going to carry out the surgery had looked at the evidence and decided that I was an emergency case. If I did not have the operation very soon, the danger was that my colon could get completely blocked and I would not be able to go to the toilet at all, despite my refined diet. The team were, therefore, going to bring everything forward and I was requested to go into hospital on Friday 3 November – so just two days’ notice. I would consult with the doctor, speak to a stoma nurse beforehand and have the actual operation the following day (4 November)! It was a lot to process, but I did not panic and did not have much time to think about it. A ‘family action plan’, which was already in place, suddenly kicked in. I would move into a different bedroom in the house and get set up with a brand new, comfortable bed, after years of trying to sleep on a futon in a musty, leaky attic. The timing was perfect as on the day before I left for hospital part of my bedroom ceiling fell down under the weight of recent rainwater that had bypassed the roof!
The Stoma Operation
So in the week that comedian Rhod Gilbert’s cancer documentary ‘A Pain in the Neck’ aired and on the same day (3 November) as Channel 4’s annual Stand Up To Cancer fundraiser, I went into Norfolk and Norwich University Hospital. I met with the surgeon that was going to carry out the operation and a stoma nurse with exactly the same name as a singer/songwriter I saw in Preston earlier this year. Going through the Same Day Emergency Care (SDEC) unit, I was informed that my operation was on an ’emergency’ list meaning I could be called at any time if a window appeared, but that priority was still given to those coming through A&E. I was ‘nil by mouth’ for the whole of Friday and Saturday. It was an incredibly long and frustrating wait as other ’emergencies’ pushed my operation back. Apart from a small bowl of cornflakes on Sunday morning, I went 52 hours without any food. Nonetheless, the operation to insert a ‘loop colostomy’ was carried out successfully late on the Saturday night. It was carried out by the laparoscopic (keyhole) method, leaving two small scars on my belly. I woke up in recovery at 12:15am, given some morphine and moved back to the ward to rest. In the morning, I was predictably in some pain with my first colostomy bag attached and some bleeding. Switched to codeine, I felt better by lunchtime and had a soup and sandwich – which was so welcome after my fast. But the discomfort persisted. A second hospital stoma nurse provided me another booklet, which had some practical information. The following day, the temporary bridge (rod) that holds the stoma in place was taken out by the same stoma nurse I spoke to on the first day. I was also visited by a hospital volunteer who has been living with a colostomy for four years following an emergency appointment there. Unlike me, he had no knowledge that he would be fitted with a colostomy bag until after his operation. Although mine was no surprise, it will take some time getting used to it, emptying and replacing it. Initially, for about one week, I would use ones that drain the contents, but then I would progress to closed ones that would be changed regularly – usually 2 or maybe 3 times per day.
Looking at the stoma and the attached bag, as well as the soreness and pain it had caused, left me feeling a little depressed and cranky. It had all suddenly become real. What were the insides of my abdomen doing on the outside? It felt weird to clean the stoma and to change the bag. It also took a few days before anything other than gas and blood to be excreted. When the stoma finally started working, with the intervention of some suppositories, it was actually quite distressing. I broke down and my emotions ran high. It should become second nature, but will take some time to get used to as I adapt to this new normal. It is quite a major adjustment to my life and one that I have to live with. I must not lift anything heavy and will need to be careful in what position I sleep. Abdominal exercises, as well as getting back to walking regularly, are needed to avoid getting a hernia. I am to continue for a short while on the low residue diet, but gradually reintroduce fibre and more solid foods once my stoma has settled down and is producing the goods!
It is common to be spoken to and for medical checks to be carried out by a wide variety of NHS staff, from those taking bloods to ones handing out medication and giving blood thinning injections. But I zoned in on the student nurses from the University of East Anglia. NNUH works closely with the UEA’s Faculty of Medicine and Health Sciences to train health professionals and undertake clinical research. Of course, I could not help but ask what year of study the students were in and how their education was going. I told them about my experience at UCLan and how I gained an insight into the typical assessments of a student nurse. We spoke about Reflective Narratives and Gibbs’ Reflective cycle as they apply their knowledge and experiences on placement so far to their essay writing.
Conclusion
On 9 November, I was able to leave the hospital with a pack of supplies and plenty of information. It was a relief because I have had enough of being operated on, injected, poked and tested. Clearly the oncology representative at the MDT had restated the urgency of me needing chemotherapy, so the quicker the stoma/colostomy could be created, the sooner I could start the next, arguably more important stage. I already have a date for my MRI scan on my liver – 14 November. That will be followed by a full PET-CT scan a few days later, where a low dose of radiation will be used to check the activity of cells in different parts of the body. I will report on that in my next diary entry – in December. I’m not in any rush to go back into hospital, but I think I can cope with day visits. I realise this post is probably not as educational as the first one, because it is not about recognising symptoms that can indicate bowel cancer, but about an operation to bypass a tumour. The next one will focus on the cancer treatment and the prognosis going forward.
References:
Cancer Research UK (2023). Grades and Types of Bowel Cancer. Available at: https://www.cancerresearchuk.org/about-cancer/bowel-cancer/stages-types-and-grades/. Accessed on 29 October 2023.
Crohn’s & Colitis UK (2023). Living with a Stoma. Available at: https://crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/surgery-and-complications/living-with-a-stoma. Accessed 15 October 2023.
Lovegrove, A et al (2017). Role of polysaccharides in food, digestion, and health, Critical Reviews in Food Science and Nutrition (57:2, 237-253). DOI: 10.1080/10408398.2014.939263
Macmillan Cancer Support (2023a). Making Treatment Decisions. (5th edition). Available at: https://www.macmillan.org.uk/cancer-information-and-support/stories-and-media/booklets/making-treatment-decisions
Mohammed, A. S. A., Naveed, M., & Jost, N. (2021). Polysaccharides; Classification, Chemical Properties, and Future Perspective Applications in Fields of Pharmacology and Biological Medicine (A Review of Current Applications and Upcoming Potentialities). Journal of polymers and the environment, 29(8), 2359–2371. https://doi.org/10.1007/s10924-021-02052-2
William, A. (2023a). Healing Powers of Melon. Available at: https://www.medicalmedium.com/blog/healing-melon. Accessed on 30 October 2023.
William, A. (2023b) Aloe Vera: Gut Healer. Available at: https://www.medicalmedium.com/blog/aloe-vera-gut-healer.Accessed on 30 October 2023.
Whatever cancer throws your way, we’re right there with you.
We’re here to provide physical, financial and emotional support.
© Macmillan Cancer Support 2026 © Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland. A company limited by guarantee, registered in England and Wales company number 2400969. Isle of Man company number 4694F. Registered office: 3rd Floor, Bronze Building, The Forge, 105 Sumner Street, London, SE1 9HZ. VAT no: 668265007