Introduction
This is the seventh of my ongoing series of posts about my latest adventure – being diagnosed and treated for bowel cancer. It follows on from the previous post published on here on 25 April. It covers my two most recent consultations, a treatment update, possible scenarios and a fundraising update, but does not include sections on immunotherapy research, or a look at the costs involved. This is an edited version of one that appears that on my personal blog. Most links, images and videos have been removed to comply with Macmillan's community space.
Recent Consultation
As described in the previous post, I had an in-person consultation with my main oncology doctor on 22 April. He painted a ‘mixed picture’. The CEA numbers had dropped significantly, but that was only a marker. There was noticeable reduction in the tumour sizes, and things were ‘heading in the right direction’, with no further spread to other organs. However, the new ill-defined, slightly hypointense lesion (10mm) discovered in segment 6 was a cause for concern. This is because it could be an indication that the cancer has become resistant to chemotherapy and be more aggressive than previously. Chemotherapy began on 2 January. But we have no understanding if this newer lesion appeared before chemo started and was bigger than 10mm before it got smaller. We will probably never know when it appeared, as there was too much of a gap between the November and April scans. My only hope on this is that it has been there a while and is similar in origin to the other lesions, and will also reduce in size.
Side Effects
It was noted in this meeting that I was suffering from ‘dysgeusia’, as well as neuropathy. Dysgeusia is exactly what I have had for a few months now. All food appears to have a metallic or chemical taste. I cannot taste bland food at all and stronger flavours are needed to cut through. I have not been able to fully enjoy meals as although I can just about tell the difference between flavours, everything is masked by a metallic coating on my tongue, and is probably caused by the Fluorouracil (5FU), which I have every week. Boiled sweets help, but do not reduce the sensation. Fizzy drinks are preferable to non-fizzy ones. Nonetheless, I have carried on with a similar diet and have not really changed much apart from being fully aware that I have this and is usually worse in the week after receiving treatment. Some taste sensation did return when I took a week off and will probably fade away once treatment stops. Meanwhile, the grade 1 Cetuximab rash continues, for which I take Pliazon cream and Doxycycline (which I refer to as ‘Doctor Cycling’) – an antibiotic I last took in Tanzania. This will also, hopefully, fade away once treatment ceases. Psychologically, I feel prickly and sometimes bad tempered, like I’m being attacked by needles. By this I mean that even when I am not cannulated during the week, my ‘monkey’ brain mistakenly thinks I’m waiting for an injection or infusion. The result is I’m rarely far from blowing a fuse or losing my temper, when I spill or drop something, for example. Finally fatigue – a common side-effect. Tiredness and wanting to sleep or rest has become more prominent for me as I deal with the cumulative effects of chemotherapy. This is the use of anti-cancer (cytotoxic) drugs to destroy cancer cells. Fatigue often builds up and may increase with each treatment. This has made me less likely to take on physical activities and has, at times, lowered my mood or made me feel depressed. I’ve wanted to sleep more and have done so. This has become worse since I went into the final three cycles. Targeted therapy, such as Cetuximab (which is a monoclonal antibody) can additionally cause fatigue. Somehow, I fostered a positive mental attitude once I felt treatment was apparently working. But more recently, I don’t have the same level of physical energy that I had a couple of months ago. This, too, should pass once treatment ceases, although it can take 6 months to return to ‘normal’.
Follow-up Consultation
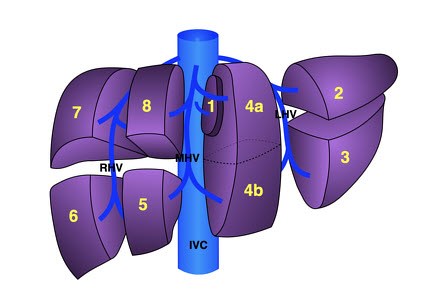
I returned on 9 May to speak with a different oncologist. Having been called a week beforehand with some indication of the results of the hepatic (liver) MDT (multi-disciplinary team) meeting with Addenbrookes, I was prepared but also nervous about the prognosis. There was ‘no comment’ from the hepatic team about risk or identification of the new indeterminate 10mm lesion. It was decided to continue with chemotherapy for three more cycles (9, 10 and 11) up until the end of June. Having asked to defer cycle 9 by one week due to the Mighty Hike for Macmillan, I was advised not to miss any more sessions over the remaining six weeks. Then I would have around four weeks off treatment as I wait for my system to clear. A PET-CT scan and another MRI scan would be scheduled for late July to determine the size of the tumours in the liver. Because of funding for Cetuximab runs out if you don’t keep up with treatment after six weeks, I might be given a further dose during this time, in case I would need to go back on this after scans. Following the scans, my case would be discussed during another Addenbrookes hepatic MDT in late July or early August. The largest metastasised tumour (53mm as of 5 April) is in the left hepatic lobe. The two, previously found satellite lesions can be found in segment 8 (right lobe, 34mm) and also in 2 (left lobe, 22mm).
The newer ill-defined, indeterminate lesion was discovered in segment 6 (also right lobe). It is currently 1cm (10mm) in diameter. So these are spread out across the liver, making a resection less likely. The chance of going to resection as of the date of this consultation is only 10-20%, but the odds may improve over the remaining 6 weeks! I am not due to have another oncology consultation until 8 August, when the results of my continued treatment, scans and the prognosis from the hepatic MDT meeting will be discussed. This is a tight turnaround so there is no guarantee at this stage if I will get an answer on that date, but that is what we are working towards.
There are three possible directions things could go in:
Treatment Update
Since the previous post, Cycle 8 was administered on 26 April and 3 May, after a week in Brighton and the first of two back-to-back consultations on 22 April, but before the second consultation on 9 May. Since January, I have missed two weeks to date – the one when I was in Brighton and a scheduled one on 10 May, due to a fundraising hike, which I report on below. Cycle 9 begun, after another one week deferment, on 17 May and was completed on 24 May. MY CEA number (see above) was down again to 13.7 – almost to a ‘normal’ level. This was similar two weeks later. A drugs supply issue meant that my treatment day shifted to Mondays for Cycle 10 – carried out on 3 and 10 June. Cycle 11 – hopefully the final one (for now) – will be carried out on 17 and (probably) 24 June. But they may insist on a final long dose on 1 July, which I will not fancy at all. Then chemo will cease (pause). The next appointment will not be until the last week of July – when an MRI and PET-CT scans will be done. I’m concerned what might happen when the chemo drugs wear off and inbetween treatment and scans. There will be up to 5 weeks before my scans, leaving me to travel a bit more – but not to Spain because of the likely temperature in July and, moreover, the prohibitive insurance cost.
Fundraising: Macmillan Mighty Hike
As previously advertised I took part in a 14.3 mile hike along the North Norfolk coast with good friends, Rene and Matthew. I missed, or rather delayed starting my ninth cycle of treatment in order to do it, otherwise I would probably not have had the energy. Together we raised £1120 for Macmillan Cancer Support. It was fairly moderate on the legs, although the 4 miles of shingle from Weybourne to Cley-next-the-Sea was a bit of a killer on the calf muscles. I managed more steps in one day than ever before, well at least since I got my smart watch in February last year. The whole event over two days, with hundreds of green-shirted participants raised over £1.1 million for the national charity, who have supported me in my journey with a travel cost grant and free counselling via Bupa. I even won £5 on their national lottery the other day. So its always good to give back. Mental Health Awareness week (13-19 May) had a theme of movement this year. But with an additional stoma, I am more than aware that movement creates ‘movement’. A grand day out! (Hope the single photo is allowed!)

Conclusion
So, despite the gloom and it being against the odds that I will proceed to a resection, I have to remain optimistic. My mood may fluctuate and my temper be short at times. I could do with getting back some of that resilience shown earlier in my treatment. It doesn't currently feel like I'm currently kicking my cancer's arse. The words ‘life limiting‘ currently haunt me. It would be somewhat miraculous if I do proceed to surgery later this year. However, I live with the small hope that I will be one of the 20% (1 in 5) who proceed to surgery from my current situation. This is because I am relatively younger than the average person with stage 4 cancer and my fitness before and during treatment. As you probably know from previous posts, I am doing everything within my control to try and beat this and allowing others to do things on my behalf. I do want a positive outcome from treatment, but as I have referred to in earlier posts I am possibly ‘playing for time’, while others are ‘praying for time’. The outcome of all this treatment to date, the scans and the hepatic MDT should be revealed sometime in August.
Whatever cancer throws your way, we’re right there with you.
We’re here to provide physical, financial and emotional support.
© Macmillan Cancer Support 2026 © Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland. A company limited by guarantee, registered in England and Wales company number 2400969. Isle of Man company number 4694F. Registered office: 3rd Floor, Bronze Building, The Forge, 105 Sumner Street, London, SE1 9HZ. VAT no: 668265007