This month is Bowel Cancer Awareness Month. Volunteer reviewer Barbara writes today's guest blog about her experience of bowel cancer. She writes about how telling her family helped her cope and about why it's important to see your doctor if you see signs of bowel cancer.
Twenty-two years ago I had bowel cancer.
I had no pain, and no piles but I lost a stone and a half very quickly, without trying. I knew something was very wrong when there was quite a lot of fresh blood in the toilet bowl. It was Christmas, and I had to wait a few days before visiting my GP.
Having nursed long ago, I suspected that the bleeding without pain was serious. Therefore I needed to see a doctor, and probably have treatment. If I guessed right, I could be out of action and hospitalised for some time. So, for me, it was logical to tell my husband that I had a GP appointment and why, and then to tell the rest of family and friends after diagnosis.
At that point I told my family about the possibilities, and of course they were all very upset. But I felt it was only fair to tell them, as they would inevitably be affected in various ways. Also, if I hadn’t told them, then my daughter wouldn’t have told her friends, and then I wouldn’t have been provided with the information that proved vital in my choosing the best treatment for me.
Apart from all this, we have a good relationship and I think they would have felt hurt if I hadn’t told them. Our children were in their early twenties at the time of treatment.
My GP referred me to a general surgeon for a check-up, and a small biopsy was taken. Meanwhile, a family friend gave me a phone number for another surgeon who did a different operation. I phoned the number and was able to attend early the next day before their regular clinic. I saw a surgeon who could perform an operation, and didn’t expect to leave me with a permanent colostomy.
Cancer was confirmed at my next attendance with the first surgeon my GP referred me to, and that surgeon suggested a permanent colostomy. So, I got back in touch with the second surgeon, and things got under way. The treatment would involve a big operation with part of the small bowel taken out and used to make a new rectum. I went up to London for the operation, and back to our local small hospital to recover.
The temporary colostomy was removed after a couple of months, and the process of getting back to normal began.
It was difficult at first, and for quite a while later, to sort out my diet. Too much fibre, and I had diarrhoea, but this slowly improved a bit. Imodium® proved useful, but needed to be taken in moderation, as it was easy to go to the other extreme and become constipated, when straining would cause piles.
This was all twenty-two years ago, and I realise how lucky I have been. The cancer being low down made it very obvious that I was passing blood, and so I could seek help in good time.
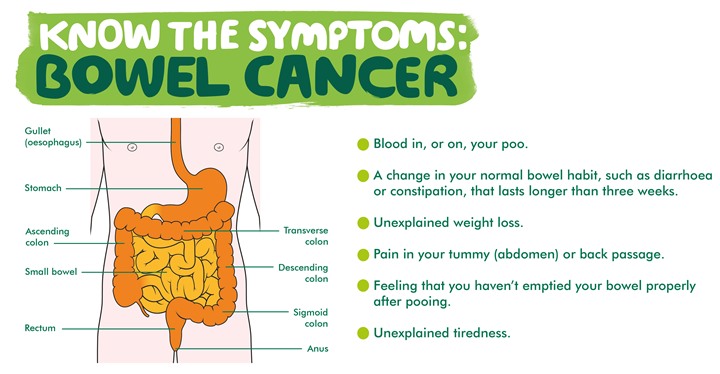
I would encourage anyone who has any of the typical symptoms (see the image below) to seek medical advice quickly, and tell family and friends why. It will also make it easier for yourself, as you may ask for help if needed, to attend appointments etc.
For me, not telling my family in particular might have caused unhappiness. I didn’t want them to think that I considered them unimportant. And, if results of tests turn up a less serious reason than cancer, then everybody can rejoice with you.
To see what else Macmillan's cancer information team has been blogging about, please visit our blog home page! You can subscribe to receive our blogs by email or RSS too.
We're with you every step of the way
The Macmillan team is here to help. Our cancer support specialists can answer your questions, offer support, or simply listen if you need a chat. Call us free on 0808 808 00 00.
Comments? Feel free to add them below (you need to be logged in).
Keep in touch Follow Macmillan’s cancer information team on Twitter @mac_cancerinfo
Whatever cancer throws your way, we’re right there with you.
We’re here to provide physical, financial and emotional support.
© Macmillan Cancer Support 2026 © Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland. A company limited by guarantee, registered in England and Wales company number 2400969. Isle of Man company number 4694F. Registered office: 3rd Floor, Bronze Building, The Forge, 105 Sumner Street, London, SE1 9HZ. VAT no: 668265007